The Health White Paper, that was tabled in Parliament in June 2023, is an important document that merits attention. Though short on specific details it does give an indication of how the government intends to handle the problems facing the national health care system.
There are several positive aspects to the Health White Paper (HWP). Firstly, it is good to have a National Health Plan. And it is commendable that the government is inviting civil society and the general public to partake in the planning of our future health care needs. The stated aspirations are matters that most people would agree to –
– the intention to build a healthy nation— for all of society, health in all policies
– a health care system (HCS) which equitable, and affordable to the public
– HCS that is resilient, affordable to the nation and has sustainable financing
– makes use of the advances in digital technology and is innovative
– optimises the use of all the health care resources in the country both in the public and the private sectors.
The HWP outlines it’s vision for the Health Care System under 4 “Pillars” which are
- Transformation of Health Care Delivery
- Prioritize health promotion and prevention of diseases
- Implement health care financing that is sustainable and equitable
- Improve the administration of the health care sector.
For the remainder on this paper I shall focus on the first pillar – Transformation of Health Care Delivery – the topic assigned to me by the Peoples Health Forum for the roundtable discussion on 7/11/2023.
Transformation of Health Care Delivery
This “pillar” is further divided into 5 components. The first is to anchor health care delivery in primary care. Every individual will be required to choose a primary health care unit – which would comprise of at least 1 doctor, one nurse and one dispenser of medicines. The PHC unit is responsible for the following
- The monitoring of the health status of all persons registered under it
- The promotion of healthy living habits in these patients – diet, weight control, exercise etc
- Screening for common non-communicable diseases
- Treatment of minor ailments at the PHC level itself
- Referral of patients to hospital for further investigation and treatment as necessary
- Follow up of patients upon discharge from hospital.
It is envisaged that the existing General Practitioners – who now number about 7500 – will be co-opted into this system of Primary Health Care units to provide the above services to their own set of patients.
The second and third components of the first pillar aim to optimize the use of the hospitals in the country. This will be achieved by
- Reducing unnecessary admissions to hospitals. Conditions that can be handled at the Primary Health Care level should be handled there.
- Patients will require a referral from their Primary Health care unit to be eligible for free treatment at the hospital level – for all the conditions specified in the “Health Benefit Package” (as yet unspecified).
- Integrating private hospitals into a national health care system. This will be done in stages, starting with the purchase of certain services from the private hospitals. At a certain stage of integration, the Primary Health Care Clinics will have the freedom to refer their patients to private hospitals, and a significant part of the charges of the private hospitals will be borne by the “Strategic Buyer”, a separate institution that will manage the Health Sector Budget.
- Electronic records will become the norm so that patients can move seamlessly through the system – from the PHC to a government or private hospital and then back to the PHC. The immediate availability of records of investigations already done, diagnoses made and treatments given will enable the attending doctor to provide optimum care.
- Hospitals, both public and private, will be organised into “clusters” so that they can share their resources including specialized diagnostic facilities, sub-speciality experts as well as beds, so as to provide good quality care in the most cost efficient manner possible.
The fourth component of the first pillar focuses on using the advances in information technology to create electronic records so that the treatment of any patient at any point in the health system will be informed by all the information available for that patient. Patients will also be given a copy of their electronic records. Tele-consulting will also be enabled so that specialist opinion can be sought even from rural and remote clinics. Finally, the data in the system can be used to assess whether specific services need to be expanded and whether new services are required.
The fifth component of the first pillar emphasizes equitable access for all sectors and strata of society. The elderly, the Orang Asli, people with disability (OKU), HIV+ve people, migrants, the stateless and refugees are specifically identified as groups that may have difficulty in accessing health care. It also recognizes the social determinants of health
Chart One: Overview of the Health Care System proposed in the Health White Paper
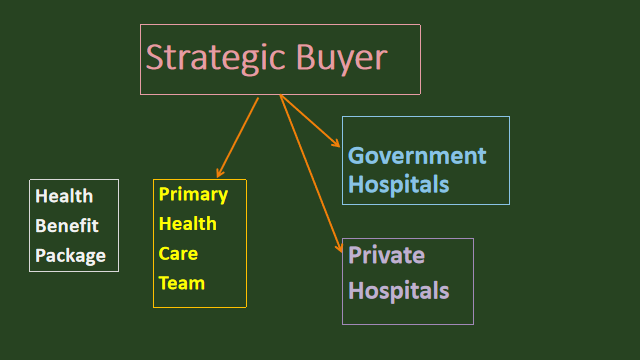
Main features
- PHC team emphasizes health promotion and treats milder complaints. It also serves as the gateway to hospital care.
- The PHC can refer patients to either public or private hospitals (depending on criteria that have yet to be specified)
- The Strategic buyer will reimburse the PHCs as well as the hospitals for treatment of conditions listed in the Health Benefit Package (yet to be specified).
The Peoples’ Health Forum’s Concerns
The objectives defined by the HWP are on the whole good. But we are concerned that the massive changes proposed to the manner health care is provided and paid for, might create significant problems that are not anticipated by the planners. Some specific concerns are as follows
- In the model outlined by the HWP, the Primary Health Clinics play a pivotal role in arranging care at the secondary and tertiary levels. Only patients who are referred by the PHC will get free health care at the next level. The exact mechanism of the referral system is not as yet specified but is very important. If there are features – financial or otherwise – that penalize PHCs for referring too many patients to secondary or tertiary care, that would create a conflict of interest between the PHC and the patients under their care.
- The HWP is advocating a major change in the financing of public sector hospitals. Currently, financial considerations are not the main drivers of clinical and administrative decisions in public hospitals. Switching to the Strategic Purchaser System where all hospitals are paid by the clinical services they provide, will alter the way health care is delivered, in a fundamental way, and not necessarily for the better. Medicine is not an exact science – the threshold for doing an appendectomy, or a caesarian section or a cardiac angiogram can be altered by financial considerations. The fee-for-services-provided system will create a tendency to over-investigate and to resort to surgery as these modalities will increase the revenue of the hospital.
The over-all cost of health care will then go up, because there will be financial incentives for hospitals to “over-diagnose” and “over-treat”. The Strategic Purchaser will also need to have a large army of employees to process claims from the various hospitals to ensure they are not over-claiming. The incidence of complications arising from medical interventions will also go up.
- The HWP talks about “financial and operational autonomy for public sector providers”. It is important to know what this means. For example, would public sector hospitals be allowed charge co-payments or to open private wards and offer services to health tourists to increase their incomes? Would public hospitals in poorer regions of the country have less revenue as they will not be able to charge much co-payments compared to hospitals in large urban centres? Will the richer public sector hospitals be able to attract and retain more qualified staff compared to the poorer public sector hospitals in the rural areas or poorer states?
- The dedicated health fund (Strategic Purchaser) will procure services in both the public and private sectors. This will essentially mean that a channel is provided for the public financing of the private healthcare sector. Will the diversion of public funds to private hospitals lead to the undermining of the public hospital system?
It is important to remember the weaknesses of the private hospitals, which either were not able to (or did not want to?) manage COVID patients. In fact, in the midst of the pandemic, private hospital spokespersons were seen to place their own financial position in front of everything else. At least one high-end private hospital chartered airplanes to bring in medical tourists from Indonesia even before the country had fully opened up, no doubt with their bottom line in mind.
The COVID-19 pandemic showed very clearly that it is imperative to have a public healthcare sector that is strong and well-resourced in these times of emerging and re-emerging communicable diseases, and furthermore, that the private hospitals cannot be relied on to put national and public interest ahead of their own financial interests.
- The HWP gives no details about the conditions and treatments that will be listed in the “Health Benefit Package”. That list is crucial because these are the treatments that the Strategic Purchaser will pay for. What happens to the individual with the rare complaint which is not listed in the Benefit Package? What happens when a new but effective modality of treatment is developed? How long will it take before it is considered for adoption to the Benefit Package?
With the advancement of technology, medical imaging and treatment is going to get increasingly expensive. Every health care system will require to institute some form of rationing. The question is how open and democratic that process of rationing is going to be.
- There is no in-depth discussion of how weaknesses in the monitoring and regulation of the private medical education sector resulted in an oversupply of doctors and paramedics, some of whom are not adequately trained. The issue of “regulatory capture” of the regulatory bodies by large corporations providing medical education is not identified. A discussion of how regulatory capture can be minimised is crucial if we want to ensure a similar “capture” of the proposed “National Health Fund” by the private hospitals and the pharmaceutical industry does not take place.
- Electronic records and the question of confidentiality. Will commercial interests be able to buy access to patient records to be able to advertise particular products to particular people? How about insurance companies using this information to risk stratify the individuals applying for health or life insurance?
- There are strong hints within the HWP that the general public would have to pay more towards health care, though the mechanism is not specified – whether it is via a payroll tax, social health insurance or GST. The Peoples’ Health Forum (PHF) is against this idea as there is significant wage suppression in Malaysia. Our wages are ⅙ that of the advanced countries. Stunting among 5 year olds is about 20% – this means that the poorest 20% of families in Malaysia are already unable to provide for the basic nutritional needs of their children. It would not be fair to add to their economic burden by incurring an extra tax on them.
Also, the positive externalities of subsidised health care should not be under-estimated. It enhances social solidarity and a sense of belonging to the nation.
The Take Home Message
The reason why the Peoples Health Forum is organizing this roundtable discussion is because we believe that the Health White Paper is an important milestone in the development of the Malaysian Health Care system. It has many admirable aspirations. However, some of the suggested methods to attain these aspirations might actually lead to serious problems as sketched out in the section above.
So, it is crucially important that civil society groups participate in any future consultations organized by the Ministry of Health to ask for details pertaining to the various proposals contained in the HWP and to give feedback.
PHF’s Suggestions
- Go for incremental changes – eg start a pilot project for some GPs to be allocated NCD patients on a capitation basis. This will help decongest government clinics and also personalise and improve care for NCDs. This can be gradually expanded to other areas and more GPs.
- Start or further develop the cluster hospital concept in a few areas and fine tune the exercise.
- Reduce wastages in the procurement of goods and services. Is there a need for Bumiputra middlemen? If there still is, what are the margins that they can charge?
- Increase the federal health budget to 4% of GDP in stages over 5 years. That will give the MOH the necessary time to upgrade its programs.
- Make medium term and long term plans to increase Federal Government Revenue from its current 15% of GDP.
- Ensure that large commercial interests and professional groups that stand to gain financially from the further “marketization” of the Malaysian Health Care Sector, do not hijack the efforts to improve this sector.
Jeyakumar Devaraj
Chairperson
Parti Sosialis Malaysia
