Contents of Memorandum Submitted to Minister of Health on 10th March 2025
PSM greatly appreciates the public health-care system provided by the Malaysian Government at an expenditure of RM 46 billion in 2025. To us, the public health system is the actualization of the motto “a caring society” and it makes our country a more compassionate one. It is more than just an essential service. It serves as a glue that binds us together and consolidates our common identity. In a very real way, it defines the “soul” of the nation! This public health-care system must be defended and strengthened, so that it can continue to provide high-quality services to our people regardless of their economic status or their ability to pay.
However, we are alarmed by some of the statements emanating from our political leaders and senior officials from the Ministry of Health, as these seem to indicate a departure from the principles of universal health care towards a new system with elements of commercial calculations. Among the issues that have raised these concerns are:
1. Recommendations for the establishment of a “Strategic Buyer” agency.
According to the proponents of this recommendation, which includes the Parliamentary Special Committee on Health-care, the role of the Strategic Buyer is to pay for the cost of treatment both in government hospitals and private hospitals. One of the objectives of this proposal is to integrate the public and private treatment systems so that all citizens can benefit from the expertise that exists in both sectors.
However, to implement this proposal, all government hospitals will have to be corporatized, so that they can function as a company and apply for reimbursement from Strategic Buyer for each patient they treat – thus competing on a “level playing field” with their privately owned counterparts. This envisages a major change in the way government hospitals are funded. Currently, government hospitals receive a “global budget” based on their expenditure for treating patients the previous year. The new funding system requires public hospitals to submit charges for each patient they treat. This will change the way patient care is practiced in government hospitals (because the new system will force government hospitals to act like businesses) and is likely to create the following problems –
– a tendency to give more serious diagnoses because they elicit larger payments from the fund. For example, a diagnosis of “unstable angina” will get a bigger payment than a diagnosis of “chest pain for investigation”.
– will lead to the lowering of thresholds for interventions, such as angiograms for chest pain, appendicectomy for patients with abdominal pain and LSCS surgery for pregnant women, because hospitals can charge more for interventions.
– the likelihood that this new funding system that activities that do not much financial compensation, such as health education, preventive measures, screening for NCDs, etc will tend to be neglected.
– will increase management costs because each case must be claimed from the Strategic Buyer. Bureaucracy will increase dramatically. The cost of auditing to prevent fraud by claimants will also increase costs.
But the biggest negative impact is that the ethos in public hospitals will change towards a business ethos. The current ethos is more holistic and based on clinical needs. The issue of cost and how to increase the amount to be claimed from Strategic Buyers will become dominant if public hospitals are corporatized. That will alter the way medicine is practiced in Malaysia – and not in a positive or wholesome direction.
2. Rakan KKM Scheme
PSM is not comfortable with this scheme because, we estimate that, in Malaysia, approximately 70% of the specialists with more than 10 years of experience after becoming a specialist, are in the private sector, while 70% of the of patients requiring in-patient treatment, are treated in public hospitals. The shortage of specialists in the government sector is the main cause for the long waiting list for appointments to see specialist doctors, delays in scheduling angiograms, surgeries and other such interventions, dissatisfaction among the public, and mental stress and the phenomenon of “burn-out” among government doctors. Specialist shortages is a “core” problem!
The implementation of Rakan KKM will cause this imbalance to become worse because a portion of senior specialist doctors will be involved in this scheme, and their time to care for non-paying public patients will be reduced.
Inadequate Allocation for KKM
In our understanding, both the above schemes have been proposed because of the long-standing under-allocation of funds for the Ministry of Health (MOH).
We are aware that the Ministry of Health receives the second largest allocation among government ministries. The allocation for the MOH for 2025 is RM 46 billion or almost 12% of the total national budget. But to us, this is not enough. Developed countries are allocating approximately 19% of their budgets for the public health care system as recorded in the table below.

Our recommendation is that Malaysia should increase its allocation for public health services to 5% of GDP within 5 years.
We are well aware that the Malaysian Government is currently saddled with a debt of RM 1.2 trillion (or about 62% of GDP), and that the deficit in the 2025 budget is approximately 4% of GDP. But it is important to step back and ask ourselves why this should happen in a country that has experienced GDP growth of 3% to 8% per annum for the past 30 years (instead of opting for market driven measures which, in the final analysis, have created many of the problems in the first place). .
The following chart summarises our analysis –
Chart One: Real GDP Growth 1970 -1999
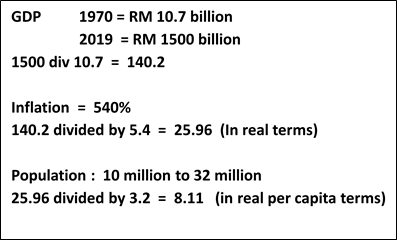
As illustrated in the calculations above, which are based on official government figures), the GDP in real terms (i.e. after taking into account the effects of inflation) in December 2019, was 26 times greater than in 1970. However, Government revenue, measured as a percentage of GDP, declined from 30% of GDP in the 1980s to 16% of GDP today, as reflected in the chart below.
Chart Two: Federal Government Expenditure as % of GDP
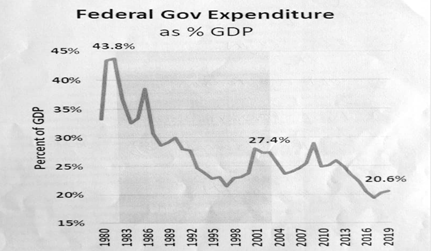
(Chart presented by Dr Dzul during his first term as Health Minister)
The main reason for this phenomenon (which is replicated in almost all countries in our world) is that corporate tax in Malaysia, which is the main source of government revenue for Malaysia, has been reduced in stages from 40% of profits in 1988 to 24% of corporate profits this year. Malaysia is engaged in a “race to the bottom” with our ASEAN neighbors as we compete for foreign investors. Corporate tax in Thailand is currently 20% of corporate profits, and it is only 17% in Singapore.
This race to the bottom is not destined by God. (Though it is recommended and encouraged by the World Bank and the IMF.) Why are we not engaging in a dialogue with our ASEAN neighbors to stop this race, which is severely restricting the capacity of our governments to care for the people and to mitigate climate change? This is PSM’s question to the Madani Government and also to the governments of neighboring countries.
In our view, any attempt to shift the financial burden onto the shoulders of ordinary people through compulsory salary deductions to fund health expenses, or through taxes such as the GST, is irresponsible in a country where wages have been pushed to a low level – electronics factory workers in Bayan Lepas enjoy wages that are only one-eighth the wages of electronics factory workers in California even though the machines and technology they use are the same. There is severe “wage suppression” in Malaysia and other ASEAN countries.
According to the PSM’s calculation, the distribution of national income is as shown in the chart below –
Chart Three: Distribution of National Income in Malaysia 2024

We are not naïve. We understand that if Malaysia increases corporate tax unilaterally, there is a real possibility that investors will move to neighboring countries and job creation in our country will plummet. However, if the increase in corporate tax can be synchronized with Thailand, Indonesia, Vietnam and the Philippines, the negative impact on our economy can be minimized.
Has this concept been brought up for discussion among Malaysia’s political leaders and economic planners? Agreed, this proposal will be a hard sell – it will take time to gain consensus among ASEAN countries. But has the effort to discuss this important issue even begun? This is the PSM’s question to the Madani Government.
Migration of Specialist Doctors to Private Hospitals
We agree that this is a major problem and that it exacerbates the imbalance between specialists and patients in the public sector compared to the private sector. PSM’s recommendations to address this crucial issue are –
a) A moratorium on the construction of new private hospitals for the next 10 years. Because, every time a new private hospital starts operations, the senior managers of the hospital will persuade dozens of specialists serving in government hospitals to move to the new private hospital. Not only specialist doctors, but also trained nurses from the operating theatre and ICU, technologists from the laboratory, cardio unit, x-ray department and other units will be persuaded by the private hospital managers to resign from their positions in public hospitals and work in private hospitals.
A moratorium on new private hospitals will greatly assist the Ministry of Health fill up the vacancies for specialists, trained nurses and medical technologists so that the quality of health services offered to our people can continue to improve. This might impair (a bit) the profits of the GLCs that own several private hospital chains (they certainly will not go bankrupt because of this). But what are our priorities as a nation? Isn’t the well-being of our people more important than the profits of GLCs?
b) Creation of Special Service Commission for MOH Staff
The military, Ministry of Education and the Judicial System have their own Service Commissions. Why can’t MOH, with more than 300,000 staff, have its own service commission? Our additional recommendation would be to use the service scheme at the National Heart Institute as a template to for the terms of service for MOH staff.
Civil Medicine Scheme (Skim Perubatan Madani)
This scheme, launched in July last year in ten districts, provides funds for the population to go and see private clinics free of charge. The objective is to reduce the severe congestion in the government facilities in these districts. So far 2.5 million patients have been diverted to the GP Clinics.
We welcome the government’s approach to think outside the box. But we think it would be better if this scheme could be modified to enhance the quality of follow-up for patients with NCDs such as diabetes, high blood pressure, gout and asthma by offering them a personal doctor.
The PSM proposal is to offer patients with NCDs, follow-up with a private clinic near their home for free. The General Practitioners (GPs) who participate in this scheme will be paid a capitation fee for each NCD patient they care for. Private clinics will not charge any fees for these NCD patients and will be supplied with medicines free of charge by MOH. The cost of blood testing will also be borne by the government. The patients opting for this scheme will benefit from shorter waiting times and more personalized treatment.
Private clinics participating in this scheme should be required to follow SOPs to care for patients with NCDs in terms of blood pressure monitoring, weight, blood tests and health education. Better follow-up of NCD patients will prevent complications and thus increase health status, and reduce health care costs in the long run.
The capitation fee paid to GPs under the National Health Service (NHS) system in the United Kingdom is approximately RM 24 per patient per month. This fee is paid to the clinic whether or not the patient visits the clinic that month. The fee for GPs in Malaysia should be determined through discussions with the private doctors’ union.
PSM’s recommendation is to launch this program in one or two districts as a pilot project to study how it can be implemented more widely without problems.
Closing Comments
We would like to express our sincere gratitude to the Ministry of Health and the YB Minister of Health for this opportunity to share our views and recommendations. We are always ready to work with the Ministry of Health in improving the quality of health services in our country. As we have said earlier, the public service system in our country is a national asset that must be preserved, and protected from business influence. We would also like to take this opportunity to record our appreciation for the efforts and sacrifices of all the Ministry of Health staff in carrying out their noble duties. You make Malaysia a better place.
